The menstrual cycle is a vital aspect of female reproductive health. Understanding how it works can help you better manage your health, plan for pregnancy, and recognize any potential issues that may require medical attention.
What is a Normal Menstrual Cycle?
A menstrual cycle is the regular, natural changes in the female reproductive system that make pregnancy possible. The cycle is counted from the first day of one period to the first day of the next period.
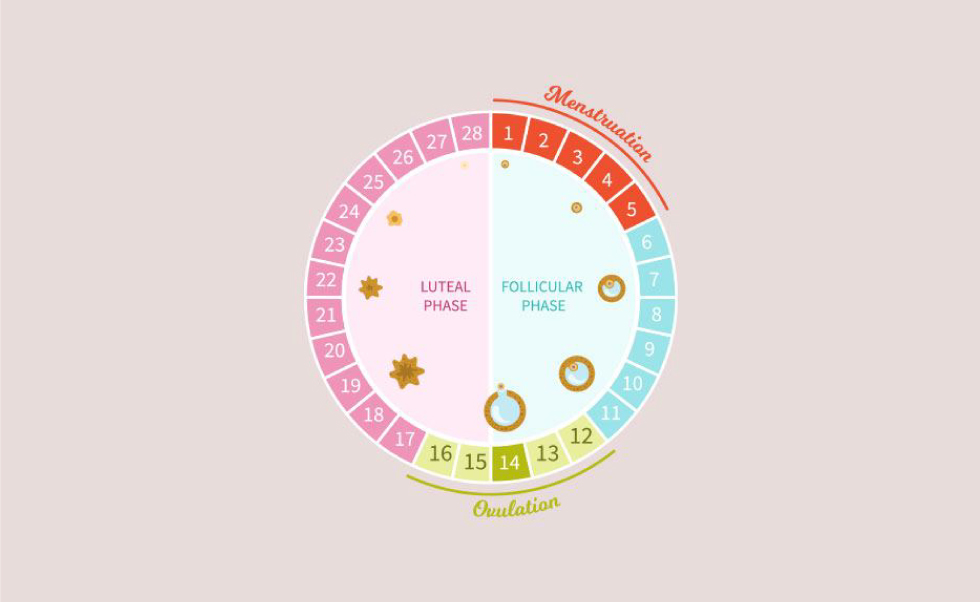
A typical menstrual cycle lasts about 28 days, ranging from 21 to 35 days in adults and 21 to 45 days in young teens. The cycle consists of four main phases: menstrual, follicular, ovulation, and luteal.
The Four Phases of the Menstrual Cycle
- Menstrual Phase (Days 1-5):
- The menstrual phase starts on the first day of your period and lasts about 3 to 5 days. During this phase, the thickened lining of the uterus (endometrium), which would support a pregnancy, is shed through the vagina if no fertilization has occurred. This results in menstrual bleeding.
- Follicular Phase (Days 1-13):
- The follicular phase overlaps with the menstrual phase initially. It starts on the first day of your period and ends with ovulation. During this phase, the pituitary gland releases follicle-stimulating hormone (FSH), which stimulates the ovaries to produce around 5 to 20 tiny sacs called follicles. Each follicle contains an immature egg. Usually, only one follicle will mature into an egg.
- Ovulation (Day 14):
- Ovulation typically occurs around day 14 of a 28-day cycle. This phase is marked by the release of a mature egg from the ovary into the fallopian tube, awaiting fertilization. The surge in luteinizing hormone (LH) triggers this release. This is the most fertile period of the cycle and the best time for conception.
- Luteal Phase (Days 15-28):
- After ovulation, the luteal phase begins. The ruptured follicle transforms into a structure called the corpus luteum, which secretes progesterone and a small amount of estrogen. These hormones maintain the thickened lining of the uterus, preparing it for potential pregnancy. If fertilization does not occur, the corpus luteum breaks down, leading to a decrease in progesterone and estrogen levels, triggering the start of menstruation.
What Hormonal Changes take place in my Menstrual Cycle?
The menstrual cycle is regulated by a complex interplay of hormones:
Follicle-Stimulating Hormone (FSH): FSH is released by the pituitary gland at the start of the follicular phase. It stimulates the growth of ovarian follicles and helps one follicle reach maturity.
Luteinizing Hormone (LH): LH surges mid-cycle, triggering ovulation. The release of LH causes the mature follicle to release its egg.
Estrogen: Estrogen levels rise during the follicular phase, leading to the thickening of the endometrium. It also plays a role in the regulation of FSH and LH levels.
Progesterone: After ovulation, progesterone levels rise due to the corpus luteum. It maintains the thickened endometrium, essential for supporting a potential pregnancy.
What happens during Ovulation and Fertilization?
Ovulation is the release of a mature egg from the ovary. This typically occurs around the middle of the menstrual cycle and is the most fertile period for a woman.
Ovulation can be detected by a slight rise in basal body temperature and changes in cervical mucus, which becomes clear and stretchy, similar to egg whites.
Fertilization happens when a sperm successfully merges with an egg in the fallopian tube.
this can occur within 12 to 24 hours after ovulation. If fertilization occurs, the fertilized egg (zygote) travels down the fallopian tube and implants into the uterine lining, leading to pregnancy.
What happens if fertilization does not happen?
If fertilization does not occur, the egg disintegrates and is absorbed by the body, leading to the shedding of the uterine lining and the start of a new menstrual cycle.
Importance of Understanding Your Menstrual Cycle
understanding your menstrual cycle is crucial for several reasons:
- Family Planning: Knowing your cycle helps identify the most fertile days, aiding in conception or natural birth control.
- Understanding your menstrual cycle is not just about reproduction, it’s about your overall health. Regular cycles can indicate good reproductive health, while irregularities might signal underlying health issues that require medical attention. By monitoring your cycle, you are taking responsibility for your health and ensuring you receive the care you need, making you feel cared for and responsible.
- Managing Symptoms: Understanding hormonal changes can help manage symptoms like PMS, cramps, and mood swings.
Tips for Tracking Your Menstrual Cycle
- Keep a Calendar: Mark the first day of your period each month to track the length of your cycle.
- Note Symptoms: Record any symptoms such as cramps, mood changes, or breast tenderness to identify patterns.
- Use Apps: Numerous apps help track your menstrual cycle and predict ovulation days. These apps often allow you to record your period start and end dates, track symptoms, and predict your fertile window based on your cycle history.
Understanding your menstrual cycle is not just informative, it’s empowering. It puts you in control of your reproductive health, allowing you to plan for pregnancy, recognize normal versus abnormal changes, and maintain overall well-being. By being aware of the phases, hormonal changes, and the process of ovulation and fertilization, you can confidently navigate your reproductive journey. Regularly tracking your cycle and consulting with a healthcare provider for any concerns can ensure you stay informed and proactive about your health.